Alzheimer’s Disease: The Clot Thickens

Strickland, Sidney
Alzheimer’s disease (AD) is a neurodegenerative disorder that leads to memory loss and death and that affects a large and growing portion of the population. The β-amyloid peptide (Aβ) has been implicated in AD by analysis of genetic mutations linked to early onset cases of the disease. However, the mechanism of how Aβ contributes to cognitive decline is unknown. Substantial evidence suggests that AD has a vascular component: 1, AD patients often have Aβ deposits in blood vessels, called cerebral amyloid angiopathy, which provoke degeneration of the vessel wall and affect cerebral blood flow; 2, Epidemiology links vascular diseases such as stroke, atherosclerosis, atrial fibrillation, and hypertension with an increased risk for AD; 3, There is decreased and altered cerebral blood flow in AD patients; and 4, Chronic brain hypoperfusion is associated with the development of AD. Thus, circulatory deficiencies could play an important role in AD pathogenesis, with neuronal loss and memory deficits caused by vascular problems.
Elevated fibrinogen levels are correlated with increased risk for AD, and fibrinogen accumulates in the extravascular space in this disease. Previous studies from the Strickland lab showed that fibrin(ogen) deposition potentiates the increase in blood brain barrier permeability and neurovascular damage seen in AD mice. Now they have found that Aβ associates with fibrinogen in AD, altering hemostasis: fibrin clots formed in the presence of Aβ are structurally abnormal and resistant to degradation. Also, fibrin(ogen) is observed in blood vessels positive for amyloid in mouse and human AD samples, and depletion of fibrinogen lessened blood vessel pathology and reduced cognitive impairment in AD mice.
Based on these data, the Strickland lab has proposed that in the presence of Aβ any fibrin deposits formed would be more persistent, provoke aberrant hemostasis, and lead to compromised blood flow, increased inflammation, and cognitive decline. Their results suggest that one important contribution of Aβ to AD is via its effects on fibrin clots, implicating fibrin(ogen) as a potential critical factor in this disease. Therefore, exploring this association in detail will allow a better understanding of the mechanisms of AD pathology.
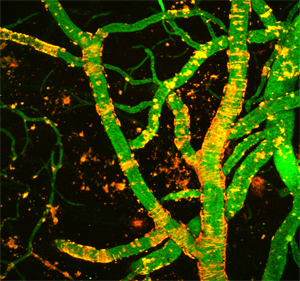
The images were taken using a multiphoton microscope and illustrate the vasculature of an Alzheimer's disease mouse. Green shows blood flow and red amyloid deposition. The ring-like structures surrounding the blood vessels represent cerebral amyloid angiopathy.
One aspect of the proposed mechanism is that it could be specifically targeted therapeutically. A drug that interferes with the effects of Aβ on fibrin clot formation would in theory normalize any blood clots formed in the brain and increase their lysis, hence improving cerebral blood flow and neuronal function and survival. Such a drug would have little effect on general clotting in other locations where Aβ levels are low. Therefore, this approach, perhaps in conjunction with other strategies, could have significant therapeutic benefit for the treatment of AD.
More generally, Strickland investigates various neuropathologies using mouse genetics, cell biology, and biochemistry. Strickland and coworkers have studied disorders including stroke, anxiety and depression, fetal alcohol syndrome, cocaine addiction, drug withdrawal, and seizure disorders.
Strickland received the BS from Rhodes College (1968) and the PhD from the University of Michigan (1972). He came to Rockefeller in 1973 as a research associate and was named assistant professor in 1975 and associate professor in 1980. He moved to the State University of New York, Stony Brook, in 1983 as an associate professor and was promoted to professor in 1987. He returned to Rockefeller in 2000 as head of the Laboratory of Neurobiology and Genetics and dean of graduate and postgraduate studies. He was named a John Simon Guggenheim Fellow in 1998, and was an established investigator for the American Heart Association from 1981 to 1986. Strickland received an honorary degree in 2006 from Rhodes College, a distinguished alumni award in 2002, and a distinguished graduate award from the University of Michigan in 2001.
Selected Publications
Tsirka SE, Gualandris A, Amaral DG, and Strickland S. Excitotoxin-induced neuronal degeneration and seizure are mediated by tissue plasminogen activator. Nature, 1995, 377: 340-344
Tsirka SE, Rogove AD, Bugge TH, Degen JL, and Strickland S. An extracellular proteolytic cascade promotes neuronal degeneration in the mouse hippocampus. J Neurosci, 1997, 17: 543-552
Chen Z-L and Strickland S. Neuronal death in the hippocampus is promoted by plasmin-catalyzed degradation of laminin. Cell 91, 1997, 917-925
Pawlak R, Magarinos AM, Melchor J, McEwen B, and Strickland S. Tissue plasminogen activator in the amygdala is critical for stress-induced anxiety-like behavior. Nat Neurosci, 2003, 6: 168-174
Paul J, Strickland S, and Melchor JP. Fibrin deposition accelerates neurovascular damage and neuroinflammation in mouse models of Alzheimer's disease. J Exp Med, 2007, 204: 1999-2008. http://jem.rupress.org/cgi/reprint/204/8/1999
Chen Z-L, Yu H, Yu W-M, Pawlak R, and Strickland S. Proteolytic fragments of laminin promote excitotoxic neurodegeneration by up-regulation of the KA1 subunit of the kainate receptor. J Cell Biol, 2008, 183: 1299-1313
http://jcb.rupress.org/cgi/content/abstract/183/7/1299
Dhadialla PS, Ohiorhenuan IE, Cohen A, and Strickland S. Maximum-entropy network analysis reveals a role for tumor necrosis factor in peripheral nerve development and function. Proc Natl Acad Sci USA, 2009, 106: 12494-9.
Cortes-Canteli M, Paul J, Norris EH, Bronstein R, Ahn HJ, Zamolodchikov D, Bhuvanendran S, Fenz KM, and Strickland S. Fibrinogen and beta-amyloid association alters thrombosis and fibrinolysis: a possible contributing factor to Alzheimer's disease. Neuron, 2010, 66: 695-709.
Further Reading
Strickland S. Tissue plasminogen activator in nervous system function and dysfunction. Thromb Haemost, 2001, 86: 138-143
Akassoglou K and Strickland S. Nervous system pathology: The fibrin perspective. Biol Chem, 2002, 383: 37-45
Pawlak R and Strickland S. Tissue plasminogen activator and seizures: A clot-buster's secret life. J Clin Invest, 2002, 109: 1529-1531
http://www.jci.org/articles/view/15961/pdf
Melchor JP and Strickland S. Tissue plasminogen activator in central nervous system physiology and pathology. Thromb Haemost, 2005, 93: 655-660
Cortes-Canteli M and Strickland S. Fibrinogen, a possible key player in Alzheimer's disease. J Thromb Haemost, 2009, 7: 146-50.
Links
Sidney Strickland, Laboratory of Neurobiology and Genetics
http://www.rockefeller.edu/labheads/strickland/
National Institute of Neurological Disease and Stroke
http://www.ninds.nih.gov/